I had the pleasure of attending the 2022 AHIP Conference in Las Vegas two weeks ago. The conference focused on creating and strengthening alliances between patients, providers, and payers to address data insights and interoperability, advance digital health, tackle social care and health equity across diverse and at-risk communities and improve physical and mental health delivery. The themes of driving towards total person care and an integrated care delivery workflow resonated loudly from many presentations.
Some presentations identified the challenges and missteps in interoperability, digital health, health equity, and integrated care delivery exposed by the COVID19 pandemic, using our shared experiences from the last two and a half years as the rallying cry for what an ideal future state might look like.
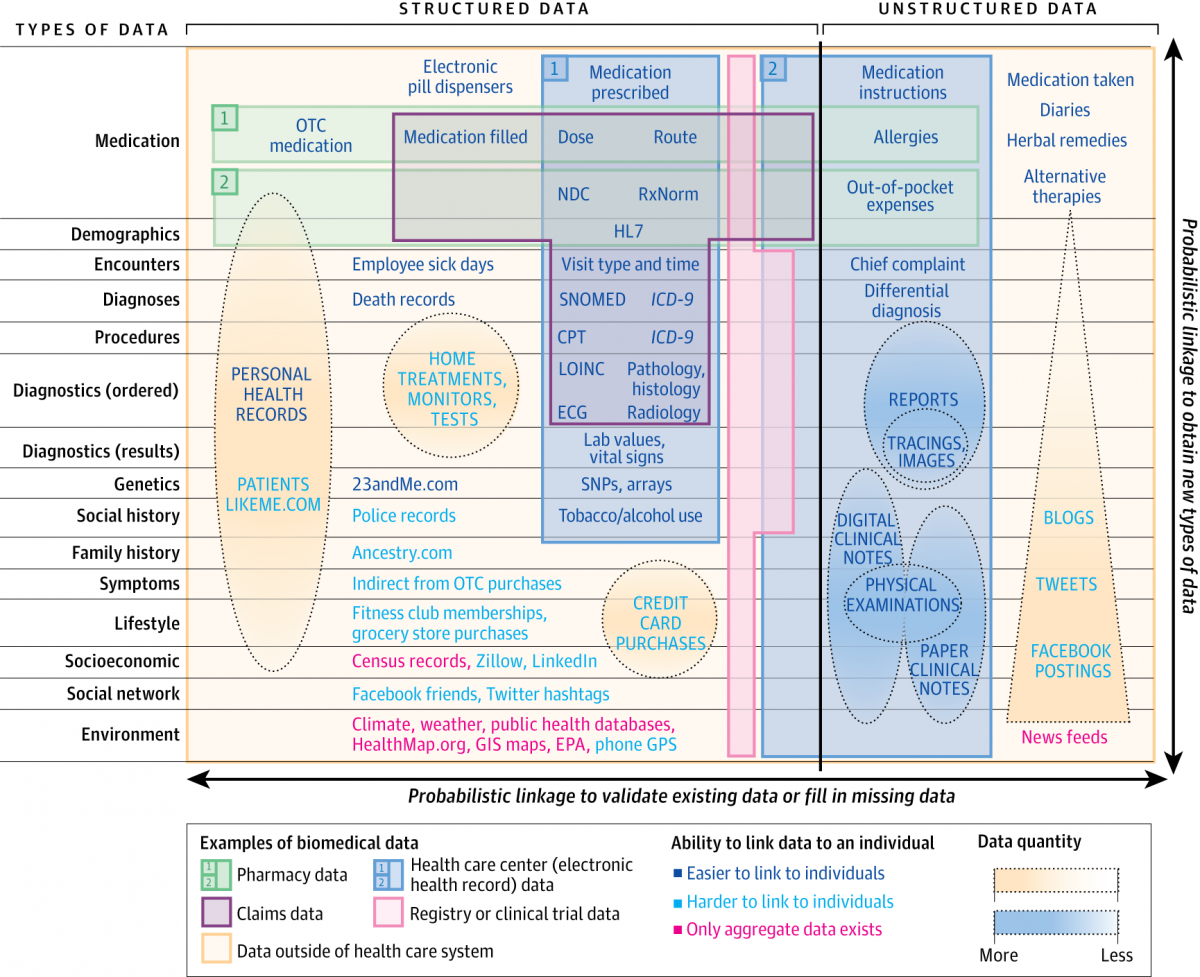
I was fortunate to present alongside Centene’s Chief Innovation Officer, Dr. Darren Schulte. Our mission was to highlight how the marriage of data from:
- Multiple different sources – health care claims, pharmacy records, electronic health records, registry, and clinical trial data, and non-health data
- At multiple levels of personalization – individual and population
- At various levels of structure – structured, semi-structured, unstructured
. . . could help drive the creation of a health care journey map for patients, capable of disrupting healthcare, evolving it from a law of large numbers (n of many) business to one of personalization (n of one). Payers would become care orchestrators and thereby the vehicle by which a utopian future state could be achieved.
Our talk identified that data driven, and consumer-centric decision-making has catapulted the success of smart-phone based cameras, GPS-enabled turn-by-turn directions, Netflix, Uber, and Airbnb, allowing them to corner market share from traditional cameras, maps, VHS and DVD rental platforms, cabs, and hotels because of their innovative product delivery models. In addition, we articulated that the airline industry has been able to take episodic engine-specific data, which is voluminous (a six-hour flight generates 240 TB of data from its engines alone), and marry it with weather, wind speed, interaction with other commercial flights, airport delays, etc. to provide robust, actionable insights for real-time course correction. This analogy of data-centrism, when applied to healthcare, sets up an interesting model where structured clinical data derived from claims, pharmacy, patient registry and, more importantly, electronic health record (EHR) sources could represent the engine data in the airline example and a myriad of other continuous and alternative data sets could provide the necessary insights to deliver real-time course correction for total patient care. The following graphic, published in a JAMANEtwork article, highlights just that. The gray, green, pink, and blue boxes represent the tip of the iceberg . . . the yellow box represents the art of possible.
Source: georgevanantwerp.com
While data availability and interoperability have progressed nicely in many of the previously mentioned markets, healthcare data has not enjoyed similar successes; this is over a decade beyond Meaningful Use. Interoperability has remained elusive because of inconsistent codes and display names and fragmented documentation in different EHR languages and dialects that don’t communicate and translate well. This is exacerbated by increasingly complex patient conditions and by complexities in care delivery models and payer workflows.
Centene has emerged as a leader in its ongoing transformation from simply a payer to a care orchestrator, using data and a member-first mindset in its quest to accomplish the same level of disruption in the healthcare delivery space. It has employed an enterprise approach of ingesting data once and deploying it multiple times in multiple formats to support use cases like HEDIS and quality, risk adjustment, prior authorization, utilization management, and value-based contracting.
More critically, this philosophy has improved care management and innovative care models and has strengthened the triad of payer, provider, and member through provider and member engagement. They understand that to solution this innovation, semantically normalized longitudinal views of patient journeys are tantamount. They have partnered with Diameter Health as the single source of truth when it comes to interoperability and data quality. Getting accurate, real-time, actionable data insights from available clinical data sources sets in motion the opportunity to access and address non-traditional data to fill in some of the gaps posed by clinical data’s episodic nature – this orchestrates the transformation of care journeys and evolves healthcare from the population to the personal.