Historically, health plans have relied on claims data to understand member health status and the care they receive. However, claims data suffer from lack of clinical details, missing results for the performed services and delay in availability. With increasing access to electronic clinical data due to the ubiquity of electronic health records and other sources, more plans are integrating clinical data to obtain more accurate and timely insights on members and to better support use cases such as quality reporting.
The challenge with using clinical data, however, lies in the variability and inconsistency of both documentation and capture of clinical information, which requires extensive refinement. In fact, this data refinement process is so complex and intricate that Gartner strongly recommends partnering with a vendor specializing in clinical data integration rather than building a homegrown solution.1 Diameter Health is one of a select group of vendors listed in this report.
Diameter Health began working with health plans in 2017. Since then, results from multiple customers confirm that Diameter Health technology significantly improves clinical data availability and usability in general, and for HEDIS reporting, specifically.
As shown in table 1, despite significant variation in source data quality, Diameter Health provided significant more usable data across multiple clinical domains. Notably, it exposed 20-60% more data for HEDIS-relevant clinical domains such as procedures, lab results and vital signs.
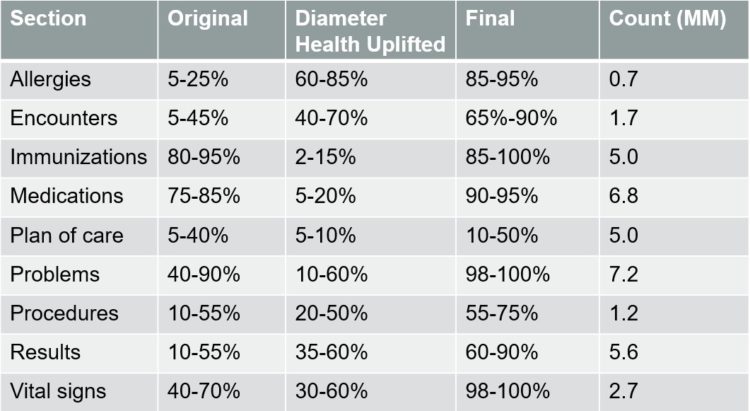
Key to Table-
- Original: Percentage of data usable from the original CCDs
- Diameter Health Uplifted: percentage of data made usable only through Diameter Health’s processes
- Final: total percentage of data usable after Diameter Health’s processes
- Count (MM): Count of clinical entries processed in the sample (in millions)
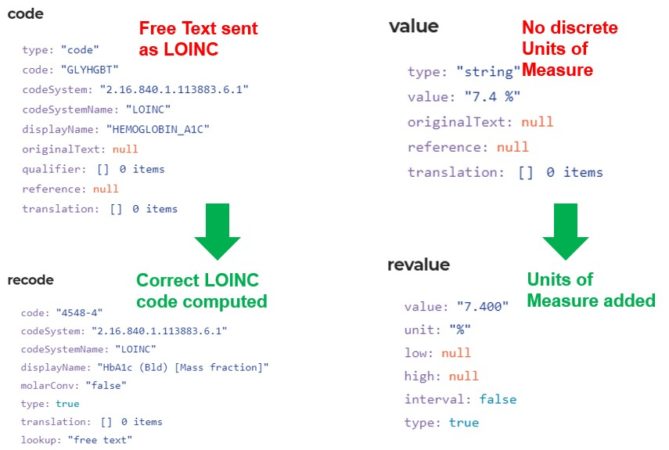
In addition, we took a closer look at several HEDIS measures particularly reliant on clinical data. We analyzed data from multiple independent payers. The results showed that, for the same diabetic patient population, Diameter Health technology consistently added 80-85% more usable “under control” HbA1c values (<9%). This substantial improvement easily translates to significant uplift in the final glucose control measure score and is consistent with our experience in reviewing tens of thousands of HbA1c results from hundreds of source systems. On average, we found that a LOINC code was not used in 40% of the HbA1c data. In another 40% of cases a proper unit of measure was not included. Consequently, an HbA1c record cannot be used for HEDIS reporting in its original format more than half the time. Diameter Health normalized the data by transforming it from its original format (e.g. free text, local code) to a standard LOINC code in the measure value set and parsing the unit, so that the data is HEDIS-ready.
We conducted similar analysis on other HEDIS measures including COL (Colorectal cancer screening), BCS (Breast cancer screening), and CBP (Controlling high blood pressure). We observed 60-80% more COL-related procedures and results, over 100% more mammogram procedures, and 10-20% more controlled blood pressure readings resulting from use of Diameter Health technology. These improvements can translate to significant improvement in HEDIS scores for these measures as well as increased reimbursement.
Health plan customers have conducted their own independent analysis of the impact of Diameter Health technology. One customer compared HEDIS-related data availability (value set matches) between Diameter Health and their own internal enterprise data warehouse. They found Diameter Health solutions provided substantial (50 – 500%) improvement across multiple HEDIS-relevant clinical domains (diagnosis, immunizations, lab results, procedures, and vital signs). Another customer submitted Diameter Health-generated supplemental data to their HEDIS engine and created impact reports. Their findings showed that Diameter Health processed data accounted for over 50% of the supplemental data matches for 40% of the HEDIS measures they reported on. The most significant impact was observed with CDC-HbA1c and childhood immunization measures, where our technology increased overall (not just supplemental data) numerator hits by double digits.
While data uplift is great for HEDIS scores, we understand that any data transformations must be consistent with the original clinical intent, and that auditors are comfortable with the transformation process. Since Diameter Health is an NCQA certified eCQM vendor,2 our technology is certified to produce standard supplemental data that can be used for HEDIS reporting without primary source verification (PSV). Even with this certification, we invest heavily in data provenance features that facilitate data tracing and validation for health plans and auditors. We also work closely with the NCQA and independent HEDIS auditors to increase their familiarity with clinical data sources as well as our technology and processes.
Clinical data availability becomes more important with new CMS regulations mandating payers to provide members API access to their claims and clinical data by mid-2021.3 We look forward to continuing our work with health plans to support HEDIS reporting and other use cases where clean clinical data makes a positive impact on both members and operating results.
References
- Healthcare Payer CIOs, Leverage Vendor Partners to Succeed at Clinical Data Integration. Mandi Bishop, initially published August, 2018, refreshed February 2020.
- https://www.ncqa.org/programs/data-and-information-technology/hit-and-data-certification/hedis-audit-and-ecqm-certified-vendor-information/
- https://www.cms.gov/Regulations-and-Guidance/Guidance/Interoperability/index